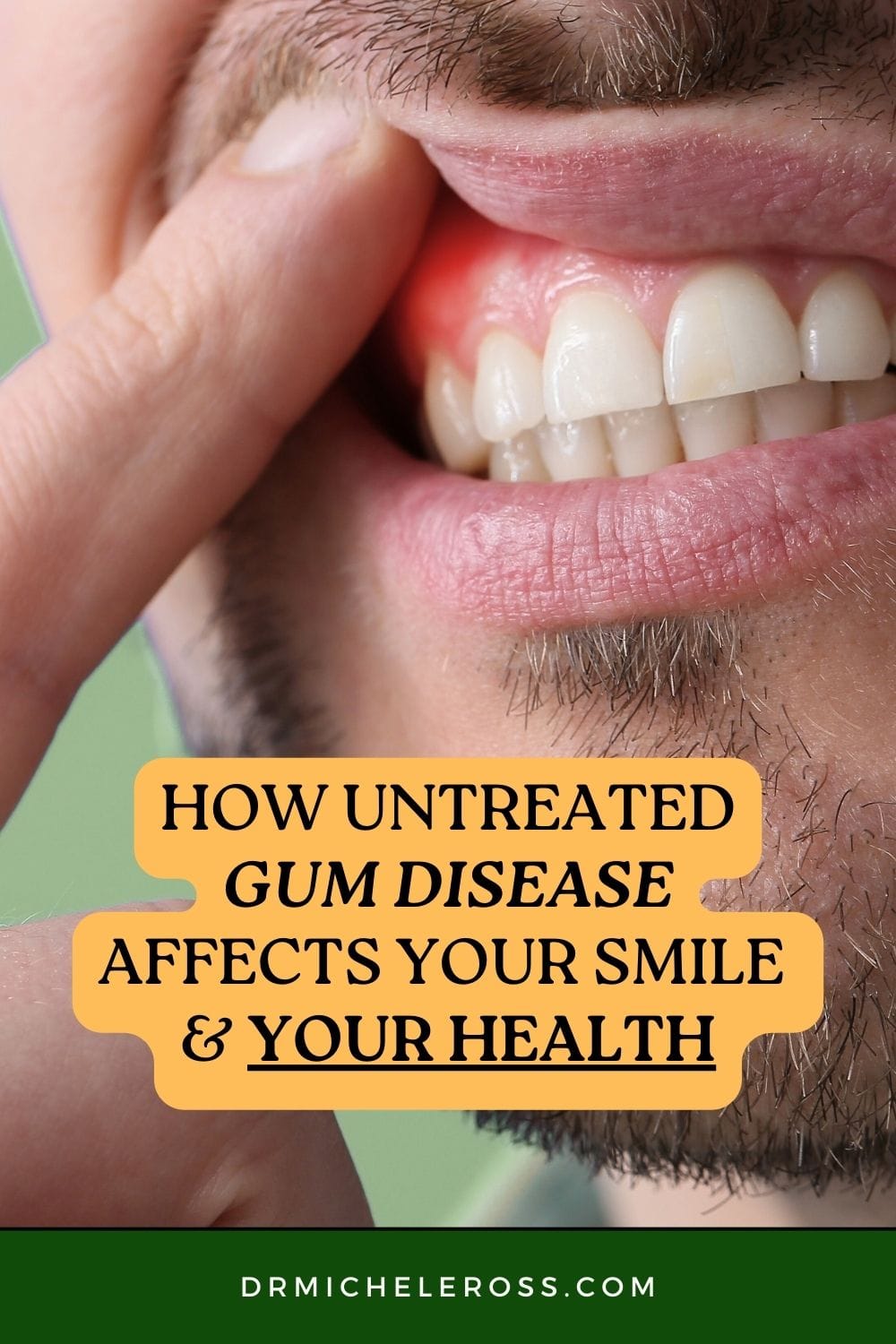
Understanding Gum Disease
Gum disease, or periodontal disease, is a persistent inflammatory condition affecting the tissues that support the teeth, including the gums, periodontal ligaments, and the jawbone. This disease most commonly starts as gingivitis, which presents as red, swollen gums that often bleed easily, particularly during brushing or flossing.
Gingivitis, while mild and entirely reversible with good oral care and professional help, is only the first step. If left untreated, it can progress to periodontitis. This advanced form is far more destructive, causing gum recession, the formation of deep periodontal pockets, and even the breakdown of bone tissue surrounding the teeth.
Without appropriate intervention, the end result may be tooth mobility and eventual tooth loss. Modern dental solutions, such as Cedar Park dental implants, offer restoration for individuals who have suffered severe consequences from advanced gum disease, ensuring both the function and aesthetics of your smile can be regained.
Addressing gum disease protects more than your smile—it is critical for safeguarding your entire body’s health. Neglecting gum disease is not just a dental oversight; it is a risk factor for systemic health complications that can impact quality of life long term.
Impact on Oral Health
The consequences of untreated gum disease on oral health are severe and multifaceted, often reaching beyond what most people might expect from an issue that starts with just minor gum irritation:
- Tooth Loss: Gum disease is the leading cause of tooth loss among adults worldwide. Bacterial infection spreads beneath the gumline and devastates the bone and connective tissues that secure teeth. Teeth may become loose, shift, or fall out entirely. This affects your ability to chew and speak and can also cause adjacent teeth to drift, altering your bite and facial structure. Losing teeth has a psychological toll, impacting self-confidence, social interactions, and career opportunities.
- Receding Gums: Gum recession is a common hallmark of periodontitis. A more sensitive tooth root is exposed as the gums pull away from the teeth. This increases vulnerability to cavities, root decay, and sensitivity to hot, cold, or sweet foods and drinks. Advanced cases require restorative dentistry and sometimes surgical grafts to replace lost gum tissue and protect tooth structure.
- Persistent Bad Breath: Chronic bad breath, or halitosis, is a common but often overlooked outcome of gum disease. Bacteria thrive in inflamed gum pockets, breaking down food debris and oral tissues, releasing foul-smelling compounds. This persistent odor can be distressing and hinder professional and personal relationships.
Connection to Heart Disease
Modern research has revealed that gum disease is not just a local issue but can influence heart health in surprising ways. Scientists believe that the chronic inflammation caused by gum disease allows bacteria and inflammatory byproducts to enter the bloodstream. Once circulating through the body, these harmful agents may attach to blood vessels, promoting the development of arterial plaque and atherosclerosis. This process has been linked with an elevated risk of heart attacks, strokes, and other cardiovascular events.
Individuals with chronic or untreated gum disease are statistically more likely to experience cardiovascular disease, and those with existing cardiac conditions may see worsened symptoms and outcomes. Restorative treatments such as dental implants Georgetown, Texas can help address severe gum disease-related tooth loss cases, supporting oral and overall health. Protecting oral health, therefore, becomes an important element of heart disease prevention.

Link to Diabetes
The relationship between gum disease and diabetes is complex and bidirectional. High blood glucose levels in diabetics provide an ideal environment for harmful bacteria to multiply, making these individuals significantly more likely to suffer from gum infections. At the same time, inflammation and infection caused by severe gum disease can increase blood sugar levels, often making diabetes harder to control.
This dangerous feedback loop can intensify complications, including delayed wound healing, greater susceptibility to other infections, and heightened risk of tooth loss. For diabetics, vigilant oral hygiene and frequent dental checkups are not just about dental appearance—they are critical components of overall disease management.
Respiratory Health Risks
Oral bacteria from gum disease don’t stay confined to the mouth. When these harmful bacteria are inhaled into the lungs, they can lead to respiratory infections such as pneumonia, especially among older adults and people with prior lung problems. Furthermore, ongoing oral infection can exacerbate chronic respiratory conditions like chronic obstructive pulmonary disease (COPD), leading to reduced quality of life and increased healthcare costs. Proper oral hygiene and regular professional dental cleanings are essential for those with vulnerable respiratory systems.
Potential Link to Alzheimer’s Disease
Recent scientific investigations suggest a connection between oral health, particularly gum disease, and brain health as we age. Researchers have identified species of periodontal bacteria in the brains of Alzheimer’s patients and suspect that chronic inflammation associated with gum disease may accelerate the onset or progression of neurodegenerative conditions such as Alzheimer’s.
While evidence is still being gathered, the prevailing theory is that persistent inflammation and the infiltration of oral pathogens can trigger wider-reaching inflammatory responses within the brain. Maintaining a healthy mouth, therefore, could play an important role in reducing the risk of future cognitive impairment or dementia.
Pregnancy Complications
During pregnancy, hormonal changes make gums more prone to inflammation and bleeding, greatly increasing the risk of developing gum disease. For expectant mothers, this is a significant concern, as untreated gum infections have been associated with adverse pregnancy outcomes, including preterm birth, low birth weight, and preeclampsia. These complications can carry serious, lasting repercussions for both mother and child.
Proactive dental care before and throughout pregnancy is crucial to reduce these risks and support healthy fetal development. Smile Builders provides useful insight into the hidden dangers of gum disease during pregnancy.
Preventing and Treating Gum Disease
Prevention is the single most effective way to fight gum disease. Building healthy habits—like brushing at least twice daily with fluoride toothpaste, flossing daily, and keeping up with routine dental visits for professional cleanings and checkups—significantly reduces your risk.
If gum disease is caught early during a dental checkup, simple non-surgical treatments such as scaling and root planing can halt the disease and often reverse its early effects. For more advanced cases with significant tissue damage, surgical interventions, placement of dental implants, or graft procedures may be necessary to restore lost function and keep the disease from spreading.
Pin This Post