Understanding Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) has emerged as one of the most effective, evidence-based treatments for depression, earning recognition from numerous professional mental health organizations worldwide. At its core, CBT is a structured, time-limited psychotherapy that empowers individuals to identify, understand, and modify negative thought patterns and maladaptive behaviors. This approach focuses on present issues and practical strategies for change, making it versatile and goal-oriented.
By helping people challenge their deeply ingrained cognitive distortions, CBT provides practical tools to foster a healthier mindset and promote emotional well-being. For those looking for support, cognitive behavioral therapy for depression offers a systematic approach that can be tailored to individual needs and lifestyles, allowing it to adapt to diverse backgrounds and unique stressors an individual might encounter in daily life.
One of CBT’s primary strengths lies in its collaborative nature. Therapists work alongside clients, guiding them through a step-by-step process to confront automatic negative thoughts, develop new perspectives, and break cycles of avoidance or withdrawal. Rather than simply offering advice, the therapist and client form a problem-solving partnership, fostering an environment of trust and mutual respect.
Through guided exercises, self-reflection, and real-world assignments such as keeping thought records or testing new behaviors in everyday situations, CBT helps individuals learn to become their own therapists, equipping them with lifelong coping skills. This self-empowerment means that even after formal therapy ends, clients can continue to use these strategies to manage stress, mood swings, or setbacks.
The Science Behind CBT’s Effectiveness
Scientific research has validated the long-term impact of CBT on brain function and emotional regulation. According to the American Psychological Association, cognitive-behavioral therapy (CBT) helps patients and families understand how thoughts, feelings, and behaviors interact, providing structured strategies to manage stress and emotional challenges. Recent findings from Stanford Medicine have shown that individuals undergoing CBT experience measurable changes in neural circuits involved in mood, impulse control, and the stress response. These neurological changes have far-reaching implications for emotional stability and improve one’s ability to bounce back from triggers that might otherwise exacerbate depressive symptoms.
CBT’s enduring effectiveness has also been highlighted in numerous clinical trials and meta-analyses, which consistently report significant symptom improvement compared to placebo or other therapeutic modalities. What sets CBT apart is its ability to create lasting, positive changes in the neural pathways that regulate thought and emotion, supporting sustainable recovery. This evidence base is why CBT is frequently recommended as either a standalone therapy or in conjunction with other treatments for depression. Furthermore, CBT encourages active participation, which improves treatment adherence and long-term maintenance of positive change. For many individuals, these long-term gains significantly enhance overall quality of life.
Key Components of CBT for Depression
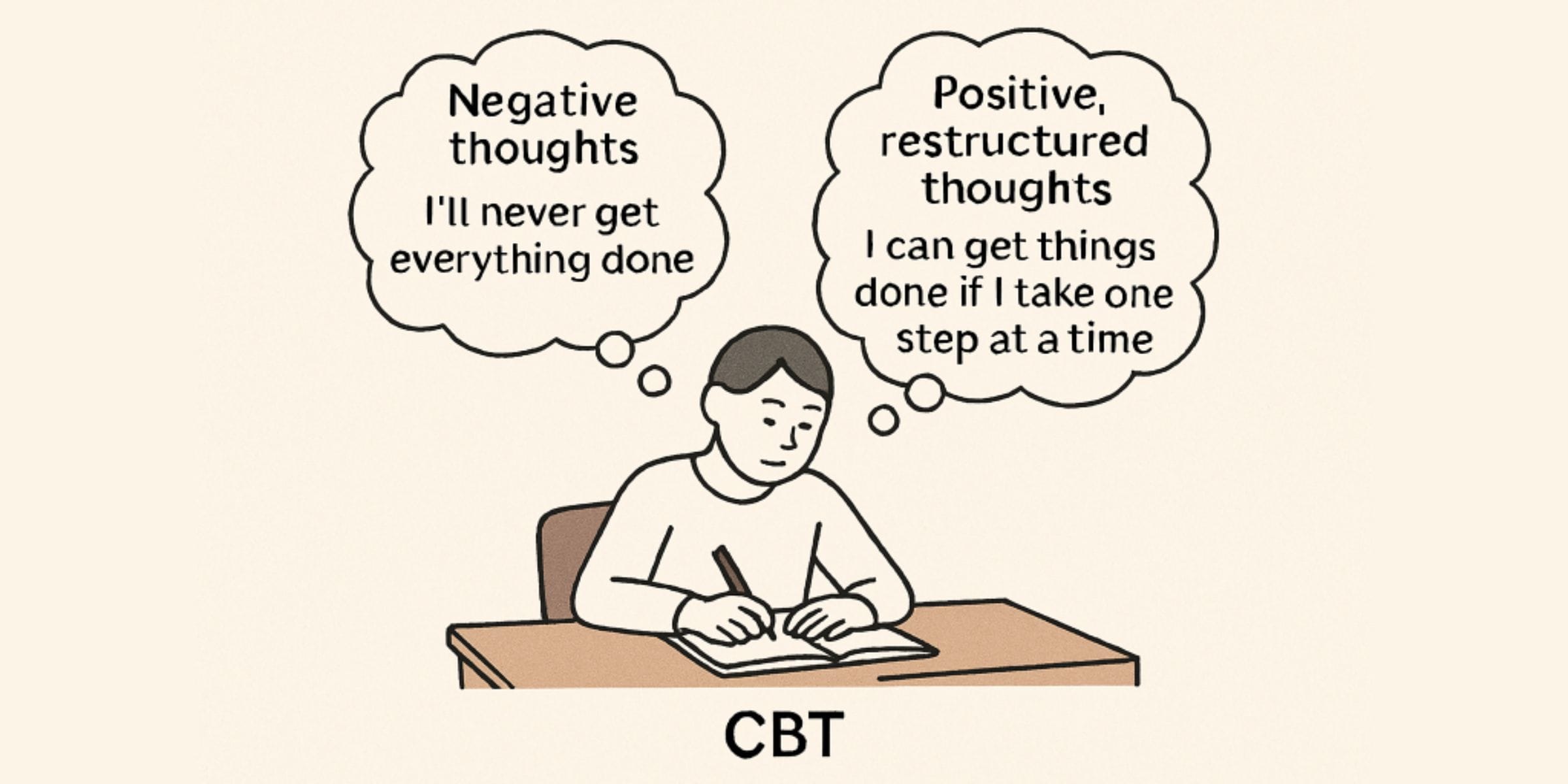
- Identifying Negative Thought Patterns: A core aspect of CBT involves learning to recognize and label distorted thoughts that fuel depressive feelings. These often include catastrophizing (“Everything will go wrong”), or black-and-white thinking (“If I fail at this, I’m a total failure”). By becoming aware of these patterns, individuals are better equipped to pause, re-evaluate, and generate more balanced alternatives that reduce emotional distress.
- Behavioral Activation: Depression often leads to inactivity and social withdrawal, which reinforces feelings of helplessness. CBT encourages gradual re-engagement with fulfilling activities, even when motivation is low, to break this negative cycle. This process might include scheduling enjoyable or meaningful tasks, taking small steps toward larger goals, or practicing social skills in safe, achievable ways.
- Skill Development: CBT trains individuals in skills such as problem-solving, assertive communication, relaxation techniques, and emotional management—tools that are essential for navigating stress and adversity. These skills help individuals respond to challenges constructively and bolster their ability to cope with setbacks or difficult emotions.
Benefits of CBT in Managing Depression
CBT offers a range of advantages that make it a preferred choice for many individuals dealing with depression. One of the most significant benefits is its focus on practical, everyday change rather than open-ended exploration of the past, which some people find intimidating or unhelpful. CBT strategies can often be practiced independently, giving individuals a sense of progress between sessions.
- Empowerment: CBT is a skills-focused therapy that encourages self-efficacy. By giving people the knowledge and tools to manage their symptoms, it fosters a sense of agency and hope. Clients learn how to intervene early when they notice signs of depression, potentially avoiding more severe episodes.
- Short-Term Commitment: Most CBT protocols are designed to fit within 8-20 sessions, depending on individual progress and treatment goals. This short-term structure makes it accessible and cost-effective for most people, while still providing sufficient depth for complex issues.
- Evidence-Based: Decades of research and hundreds of studies highlight CBT’s superior efficacy in reducing depressive symptoms, preventing relapse, and facilitating recovery. This body of research gives clients and practitioners confidence in CBT’s reliability in delivering tangible mental health improvements.
Integrating CBT with Other Treatments
For complex cases—such as those involving co-occurring depression and substance use—integrating CBT with complementary therapies can dramatically enhance treatment outcomes. People with more challenging or chronic conditions may benefit from a team-based approach that blends CBT with psychopharmacology, group therapy, or mindfulness-based interventions. CBT also works synergistically with medication and mindfulness-based therapies, providing comprehensive care tailored to individual needs. This integrated care model respects the uniqueness of each person’s journey, improving both engagement in treatment and long-term results.
Implementing CBT Techniques in Daily Life
Applying CBT principles beyond the therapy room amplifies its effectiveness. Simple techniques like “thought stopping,” where individuals consciously disrupt negative thought spirals, can be practiced anywhere and help maintain emotional balance throughout the day. Other practical strategies, including journaling, mood monitoring, and graded task assignments, can also be seamlessly integrated into daily routines for ongoing progress. According to Healthline, these exercises not only promote self-reflection and accountability but also help reinforce new habits and thought patterns. The adaptability of CBT makes it ideal for various settings, from home and work to social situations, allowing individuals to reclaim enjoyment in daily living.
Seeking Professional Guidance
While many CBT strategies are accessible through self-help resources and digital tools, working with a licensed therapist remains the gold standard—especially for moderate to severe depression. Professionals offer personalized insights, accountability, and advanced techniques tailored to each individual’s circumstances, ensuring the best possible outcomes on the path to recovery. A trained therapist can help navigate setbacks, address persistent obstacles, or modify strategies so that clients continue to grow and heal at their own pace.
Conclusion
Cognitive Behavioral Therapy represents a transformative approach to overcoming depression. By targeting the interconnected web of thoughts, emotions, and behaviors, CBT empowers individuals to dismantle the barriers to recovery, develop new adaptive skills, and experience lasting improvements in mood, outlook, and quality of life.
For anyone struggling with depression, exploring CBT could be the first crucial step toward healing and resilience. Its structured nature and focus on skill development mean the benefits of therapy can last well beyond treatment, supporting ongoing well-being and the ability to face future challenges with confidence.
Pin This Post